Research Finds Connection Between Use of Strong Cannabis and Changes in DNA, Psychotic Symptoms
Discover the latest research on the biological and mental health implications of frequent high-potency cannabis use.
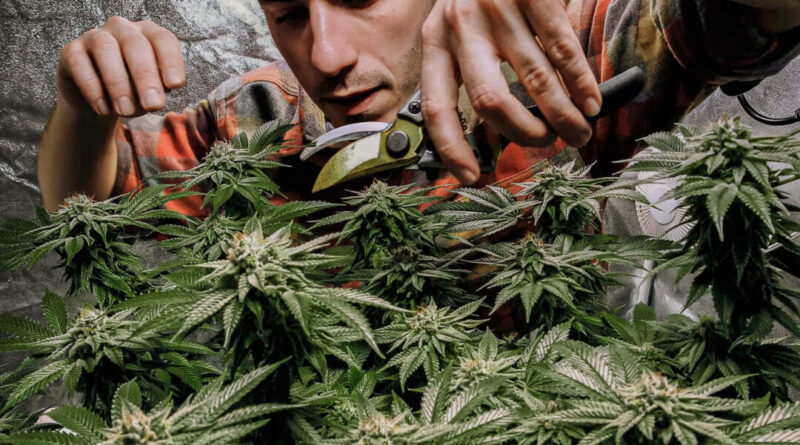
A recent study has revealed that regular use of high-potency cannabis can result in noticeable alterations in human DNA, leading to concerns about the potential mental health effects of the increasingly accessible and stronger marijuana products.
Adverse Psychological Effects Linked to Cannabis
An estimated 129 million Americans have reported using marijuana at some point in their lives, and with the legalization trends in various states, this number is expected to rise.
There is a growing body of evidence indicating the serious consequences that this trend could have on mental and physical health.
New Insights on High-Potency Cannabis and DNA
In a recent study published in Molecular Psychiatry, Di Forti and her team found that high-potency cannabis can create a distinct imprint on human DNA, demonstrating measurable biological effects of high-potency cannabis on human biology for the first time.
The study focused on DNA methylation, a process that alters gene expression without changing the DNA sequence, using blood samples from 682 participants, including 188 current cannabis users and 494 non-users.
Most frequent cannabis users reported starting cannabis use around age 16, with a preference for high-potency cannabis consumption more than once a week.
To clarify, while THC is a class of cannabinoids in cannabis, delta-9-THC is the most common form known for its potent psychoactive effects.
The study also indicated that the effects of cannabis on DNA vary between individuals experiencing their first psychotic episode and those without such experience, suggesting the potential development of DNA tests to identify cannabis users at risk for psychosis.
Co-Occurring Mental Health Issues and Cannabis Use
Mental health disorders and substance use problems often coexist. Substance use can trigger mental health symptoms, while mental health conditions can lead to substance use as a form of self-medication, according to the Substance Abuse and Mental Health Services Administration. Both share underlying causes such as genetic factors, brain changes, and trauma. Over 25% of adults with severe mental health conditions also struggle with substance use, particularly those with depression, anxiety disorders, schizophrenia, or personality disorders.
The Epoch Times consulted Dr. Matthew Sherman, chief of adult outpatient psychiatry and behavioral health at Stony Brook Medicine, regarding the connection between cannabis use and other mental health disorders. Based on his experience, co-occurring cannabis use with mental health disorders is common and often hampers treatment outcomes, he noted.
“Substances like cannabis can significantly impact treatment outcomes in a negative way,” he added, emphasizing the interactions with psychiatric medications and the effects of cannabis intoxication or withdrawal on mental health.
Ethical Considerations of DNA Testing for Psychosis Risk
Using DNA to identify risks comes with ethical considerations, as noted by Sanam Hafeez, neuropsychologist and director of Comprehend the Mind in New York City, speaking to The Epoch Times.
“This type of DNA alteration, while potentially beneficial, raises concerns about what other factors might alter our genes,” she expressed.
If DNA testing becomes more widespread, it could pose challenges for individuals with mental illness, potentially leading to misuse or unauthorized use of their DNA, legal issues, and the potential for gene modification through substances like cannabis, Hafeez highlighted.
On the contrary, Sherman expressed optimism about the potential benefits of DNA testing for patients. With appropriate tools and laboratory resources, he believes that this could be a valuable test for identifying individuals at higher risk for developing psychosis due to cannabis use.
He finds the findings intriguing, as currently, there is no method outside of clinical evaluation and risk factors like family history to determine the susceptibility of patients to psychosis.