The Impact of Fraud and Waste on Medicaid Health Services
President Donald Trump seeks to transform the federal government, in part by making substantial cuts to spending. Healthcare is a promising area for these reductions, as it constitutes approximately 30 percent of the federal budget.
In 2023, the United States allocated over $1.8 trillion to Medicare, Medicaid, and various other health programs, resulting in a budget deficit of $1.7 trillion for that year.
Medicaid alone represents $616 billion in federal expenditure, which is about 8 percent of the federal budget.
Medicaid is a joint federal and state initiative providing health coverage to approximately 80 million low-income Americans. This program is managed by the states with federal oversight, where the federal government reimburses states for a percentage of the costs incurred for each beneficiary.
In 2022, the total expenditure for the Medicaid program reached $804 billion, with states contributing 29 percent of that total—making it the largest single expense across all states.
As discussions regarding the federal budget commence, some lawmakers are suggesting modifications to Medicaid, including potential caps on reimbursement per person, reductions in state reimbursement rates, or introducing work requirements for certain beneficiaries.
Meanwhile, Trump has assured that there will be no changes to Medicaid—or Medicare and Social Security—aside from efforts to eliminate fraudulent activities.
But just how much fraud, waste, and abuse exists within the Medicaid system?
Determining the extent is challenging, as many cases of fraud remain unnoticed.
According to data from the Government Accountability Office (GAO) and the Office of Management and Budget (OMB), it seems that fewer than 3 percent of the fraudulent payments estimated have been substantiated through judicial processes. Many suspected cases may be settled out of court, and a significant amount of fraud appears to go unverified.
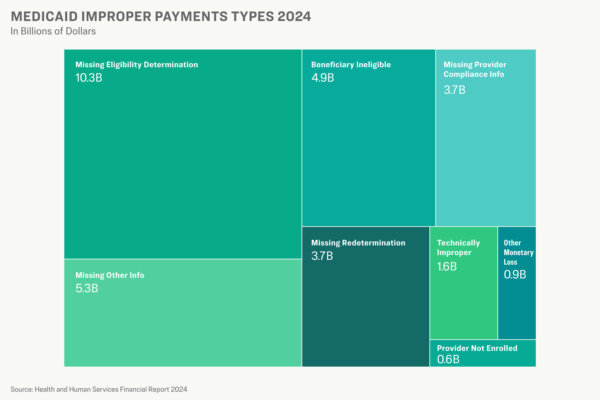
Additionally, Medicaid suffers billions in improper payments each year. In 2024 alone, these improper payments totaled over $31 billion, as reported by the Department of Health and Human Services (HHS).
A large portion of these payments stemmed from clerical mistakes, although improper payments encompass a wide range of errors, including fraud, excessive billing, and waste.
The Epoch Times has analyzed data on fraud and improper payments in the Medicaid program and conducted interviews with several current and past employees, including leaders of Medicaid Fraud Control Units from across the nation.
These sources spoke on the condition of anonymity, as they were not permitted to address the media, sharing insights about the impact of fraud and abuse on both the Medicaid program and the low-income patients who depend on medical services.
We uncovered the magnitude of the issue, the financial implications it carries, and how it affects those who need assistance the most.
Fraud
Fraud exists in Medicaid much like in all federal payment systems.
“No aspect of the federal government is immune to fraud,” states a GAO report on this topic. “We estimate that the federal government could potentially lose between $233 billion and $521 billion each year due to fraud.”
Furthermore, an OMB report indicates an average annual loss of $6.5 billion attributed to fraud over the past eight years, although this figure reflects only confirmed cases identified by a court, excluding suspected instances or those settled out of court.
The disparity between verified and estimated losses complicates the efforts to ascertain the true extent of fraud within Medicaid or any government program.
However, it is indeed an issue.
States pursue fraud cases across various types of providers, including doctors, mental health experts, and suppliers of lab services, home care, durable medical equipment, and long-term care.
Billing for services that were never provided is reportedly the most common form of fraud, according to sources speaking with The Epoch Times.
One state estimated a loss of around $2 billion to Medicaid fraud over the last five years, as disclosed by a staff member from the state’s attorney general’s office.
“These fraudsters exploited individuals in need of behavioral health services,” the staff member recounted to The Epoch Times.
The alleged wrongdoers enticed vulnerable individuals into living under subpar conditions while billing Medicaid for treatments. “They were providing little more than alcohol and shelter,” the staffer noted. Similar schemes targeting homeless populations have emerged in various states.
Kickback schemes in prescription drugs are also prevalent.
Mississippi, along with 37 other states and Puerto Rico, settled allegations related to a kickback scheme involving Biohaven Pharmaceutical Holding Company Ltd., a subsidiary of Pfizer, Inc. Pfizer agreed to pay $59.7 million, plus interest, to settle claims that Biohaven submitted false claims to Medicaid and other federal programs through cash incentives and other perks offered to healthcare providers.
Four pharmacists received prison sentences for their involvement in an international scheme that defrauded Medicaid and Medicare for prescription drugs that were never delivered, amounting to a loss of $13 million.
Hospice fraud is another widespread issue, as The Epoch Times has discovered. Patients might be enrolled in a hospice program without their consent, and when the benefits expire, their billing is rerouted to another “hospice” owned by the same provider.
Nursing homes, for instance, can defraud Medicaid by accepting funds while failing to provide adequate care for residents.
A Louisiana company managing nine nursing homes across four states agreed to a $750,000 settlement with the federal government and Maryland in 2014 to resolve allegations that it billed Medicaid and Medicare for “materially substandard and/or worthless skilled nursing facility services.”
In Mississippi alone, the attorney general’s office reported receiving 8,541 complaints relating to abuse, neglect, and exploitation of Medicaid recipients in 2024, as communicated to The Epoch Times.
Improper Payments
In 2024, Medicaid’s improper payments exceeded $31 billion, as reported by the Department of Health and Human Services (HHS). This amount includes overpayments, underpayments, and instances where it is unclear if the claims were valid.
About 74 percent of those improper payments lacked necessary documentation, such as the provider’s National Provider Identifier or confirmation that the patient had been recertified as eligible after one year.
Moreover, over $5 billion was incorrectly paid for services provided to patients who were ineligible or to providers not registered in the Medicaid system.
The Epoch Times sought clarification from the Centers for Medicare and Medicaid Services (CMS) on the percentage of improper payments in 2024 that ended up being valid after additional required documentation was submitted, but received no response before publication.
The rate of improper payments decreased to 5 percent in 2024, a drop from 8.6 percent in 2023 and significantly below the nearly 22 percent peak observed in 2021.
The figures from 2020 to 2023 were influenced by a COVID-era waiver that suspended the annual recertification requirement for Medicaid patients. According to CMS, states also improved in complying with program requirements in 2024.
The federal government reported over $161 billion in improper payments in 2024, with more than $7 billion categorized as confirmed fraud, based on OMB data.
Obstacles
Medicaid Fraud Control Units managed to recover $1.2 billion in 2023, yielding a return of $3.35 for each dollar spent, as reported by the Office of Inspector General (OIG). Investigators contend they could achieve far more with increased resources.
A shortage of personnel limits both the detection of and response to fraudulent activities. Many agencies primarily depend on tips, complaints, and referrals from other government entities to identify fraud cases. Some investigative units possess in-house data analysts or utilize data services from state agencies to detect fraudulent billing patterns.
Upon identifying fraud cases, investigators must prioritize which matters to pursue due to the constraints of limited resources. Some cases are addressed as civil matters either by the Medicaid Fraud Control Units or other state agencies, resulting in payback for overpayments but often lacking criminal prosecution.
The prosecution of fraud cases frequently encounters limitations due to a lack of resources, according to insiders who spoke with The Epoch Times. Both Medicaid Fraud Control Units and district attorneys face resource restrictions, and the cases, whether civil or criminal, tend to be intricate. Large for-profit entities can often outspend the government in defending against charges.
The complexity of the healthcare system poses additional challenges for fraud detection.
“Healthcare is immense, and navigating its billing structures is chaotic, making it challenging to pinpoint wrongdoers,” stated Neal K. Shah, CEO of Counterforce Health, which specializes in resolving health insurance claims.
Investigators liken their efforts to a game of Whac-a-Mole, as whenever one fraud scheme is dismantled, another typically arises.
Most improper Medicaid payments—those not necessarily resulting from fraud or abuse—are often due to errors made by state employees or contractors. Such errors typically stem from high turnover rates among state staff, inadequate training, or insufficient computer system checks for detecting eligibility, according to CMS. State investigators also indicate that outdated computer systems facilitating healthcare payments hinder accurate transactions and data analysis.
All these factors contribute to vulnerabilities, leading insiders to argue that the success of fraud deterrent efforts hinges on the soundness of the system. If fraudulent billing appears straightforward, the temptation for providers to exploit the system in pursuit of profit increases.
While the Medicaid program is plagued by fraud and waste, the individuals most affected are the beneficiaries.
Insiders shared with The Epoch Times harrowing stories of elderly individuals suffering in discomfort after their medications were pilfered, homeless individuals living in deplorable conditions being billed as medical care, and elderly citizens experiencing identity theft for fraudulent claims.
“You’re safeguarding public funds while also protecting the individuals who depend on receiving proper care,” an attorney working with a state Medicaid Fraud Control Unit remarked to The Epoch Times.
Regardless of any forthcoming congressional actions, the president is dedicated to enhancing the program, according to White House deputy press secretary Kush Desai.
“The Trump administration is focused on safeguarding Medicaid while eliminating waste, fraud, and abuse from the program—efforts that will enhance efficiency and elevate care for beneficiaries,” Desai communicated via email to The Epoch Times.
The Epoch Times solicited feedback from the OIG and OMB, but did not receive any responses by the time this article was published.
