Think Tank Reports Limited Improvement in Reducing NHS Waiting Times
The Nuffield Trust made the remarks after figures revealed wait times for certain treatments had increased and were not near returning to pre-pandemic levels.
Progress in bringing down NHS wait times to pre-pandemic levels has “stagnated” and long waits “remain endemic,” a think tank has said.
On Thursday, NHS England released data showing 307,500 people had been waiting more than 52 weeks to start routine hospital treatment at the end of May 2024, up from 302,589 at the end of April.
Overall, 6.38 million patients were waiting for an estimated 7.6 million pre-planned treatments at the end of May.
Though this is a relatively small increase from the previous month—when 6.44 million people were waiting for 7.57 million treatments—it’s about two-thirds higher than in February 2020, the last month before the March lockdowns and when the number of pending treatments was 4.57 million.
Not all waits had gone up. In May, 76.4 percent of patients urgently referred for suspected cancer were diagnosed or had the disease ruled out within 28 days.
This is up from 73.5 percent on the previous month and above the target of 75 percent. However, this was the first time that the goal had been exceeded since it was established in autumn 2021.
Pre-Pandemic Levels
The Nuffield Trust, an independent health think tank, said that while progress had been made in waiting times for services like cataract surgery, waits for intensive procedures had not returned to pre-COVID-19 levels.
The think tank said waiting times for hip replacements and knee replacements remained “stubbornly high” into 2023. Waiting for hip replacements, for example, rose from around 87 days before 2020 to 180 days in 2020 and for three subsequent years, median waits were around 128 days.
Nuffield Trust Deputy Director of Research Sarah Scobie said the performance figures “underline the enormous uphill battle the new government faces to get the NHS back on track.”
NHS Is ‘Broken’
A Department of Health and Social Care (DHSC) spokesperson said, “It is the mission of this government to get the NHS back on its feet, so it is there for all of us when we need it, once again.”
The spokesperson added that as a first step to cut waiting lists, the government will provide an extra 40,000 operations, scans, and appointments a week, with more clinics being open at evenings and weekends.
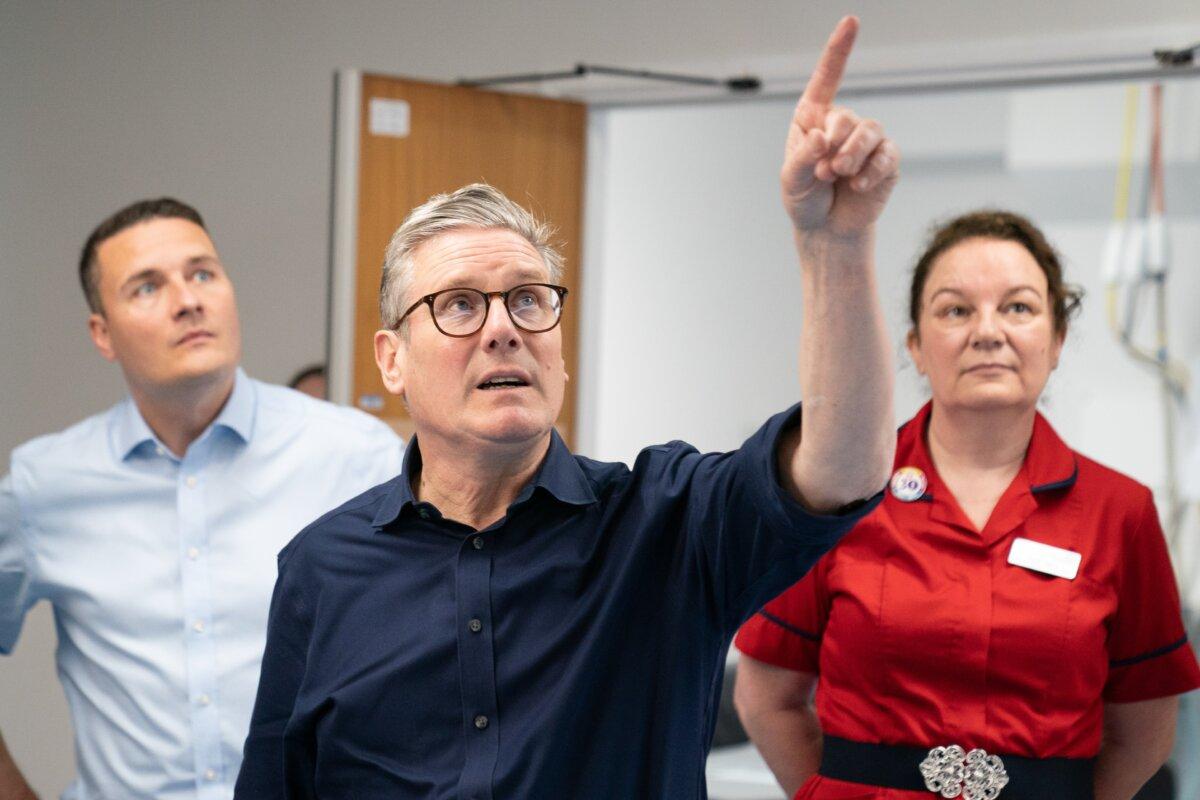
Health Secretary Wes Streeting announced that an independent investigation into the NHS’s performance would be conducted, with findings informing how the government would plan improvements.
Alternative Systems
In November, Kristian Niemietz, the editorial director and head of political economy at the Institute of Economic Affairs (IEA), rejected claims that if the NHS had more funding, it would improve.
“It is about time we started asking why it is that many other health care systems can manage perfectly fine with comparable spending levels,” he added.
Mr. Niemietz described one system where if a person gets sick they don’t pay the hospital directly, but a bill is sent to their insurer. Those insurance premiums do not depend on a person’s individual health risk, such as if they have a preexisting condition or a family history of cancer.
“It’s a system where what economists called ‘good risks.’ The people in good health, in this case, the good risks subsidise the bad risks, because they paid the same premium,” he said.
Patients ‘Gaslighted’ Over NHS Safety Concerns
The recent performance statistics and NHS review come as the patient safety commissioner—a role funded by the DHSC—said that too often, patients who had raised concerns about care had been “gaslighted, dismissed, and fobbed off.”
It was named after Martha Mills, a 13-year-old girl who died after developing sepsis in hospital in 2021. A coroner later ruled that Martha probably would have survived if doctors had responded to her family’s concerns over her deteriorating condition and had moved her to intensive care sooner.
PA Media and Owen Evans contributed to this report.





